심각한_질병이야기/Respiratory disorder
COPD Unmet medical need
Oddientist
2022. 6. 21. 16:50
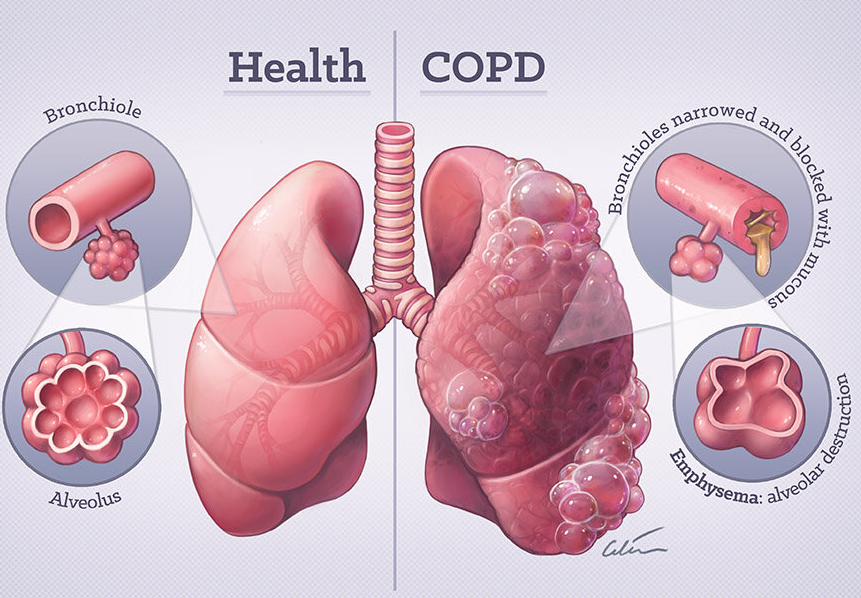
현재까지 COPD를 치료해주는 약물은 없으며, 증상 완화를 통해 환자의 Quality of life을 높이는 효과밖에 없습니다. 질병을 늦출 수 있는 방법은 현재로는 금연뿐입니다. COPD 치료에 대한 Unmet need가 무엇이 있을지 한번 알아보겠습니다.
1. Rationale for Treatment Drivers and Goals Selection
| Category | Attribute | Rationale for survey inclusion |
| 1. Efficacy | Improvement in lung function |
•FEV1, a measure of lung function, has historically been an important clinical trial endpoint for COPD drugs because it can be reliably measured and provides a robust numeric measure of lung function.
|
| Reduction in exacerbation rate |
•A clinical endpoint that has been featured in clinical trials of several recently approved therapies.
•It is especially useful for emerging therapies that target patients with more- severe disease.
|
|
| Improvement in QOL |
•Improvement in QOL is commonly measured using the SGRQ, making it a subjective measure of clinical efficacy in COPD. Without any way of stopping disease progression, physicians are often concerned about improving their patients’ QOL as much as possible, and it is often included as secondary endpoints in clinical trials.
|
|
| Improvement in exercise endurance | Hindered exercise capacity can have a significant impact on COPD patients’ QOL; as such, improving exercise endurance is a key goal of COPD treatment. | |
| 2. Safety | Rate of serious adverse event |
•Physicians balance safety and efficacy when making prescribing decisions. Thus, rate of SAEs is a key secondary endpoint in clinical trials of novel COPD treatments.
|
| 3. Convenience of administration | Delivery burden (formulation and frequency) |
•The majority of COPD therapies are delivered through an assortment of inhalers
•Patients and physicians often prefer a certain device and dosing schedule, making convenience of administration a factor driving prescribing decision
|
| 4. Nonclinical factor |
Compliance |
•Adherence to and compliance with prescribed medication impact clinical outcome.
•The variation of dosing schedule and the format of delivery route (e.g., SC, oral) of current and emerging COPD therapies impact patient compliance.
|
| Reimbursement status and out-of-pocket cost |
•COPD is a chronic condition requiring continuous drug treatment once therapy has been initiated.
•Insurance coverage varies across and within markets, and in some circumstances, patients must make substantial OOP payments.
•COPD typically affects elderly individuals, many of whom live on fixed incomes and may already incur significant healthcare expenses from managing comorbidities.
|
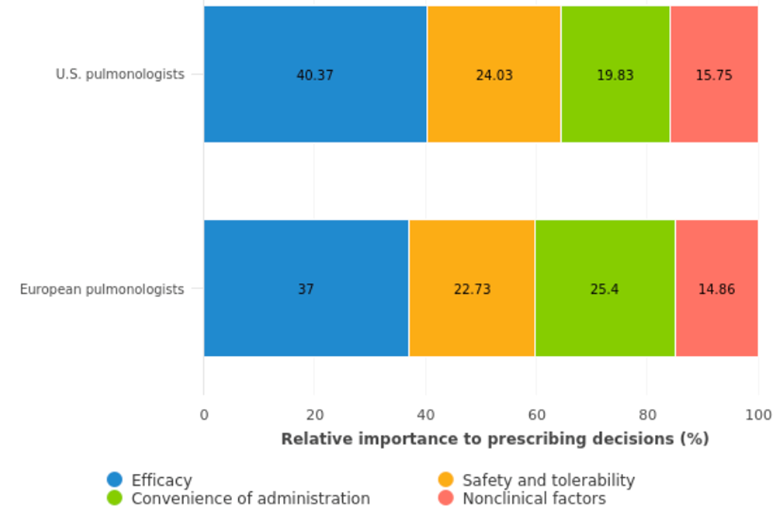
2. The key factors in treatment decisions.
- 미국과 유럽의 pulmonologists는 Efficacy를 가장 중요하게 생각했고, non-clinical factor에 대해 가장 낮은 가중치를 주었음
- Efficacy 항목 중 Reduction in exacerbation rate과 improvement in QOL는 COPD 치료에 중요한 endpoint임.
- 미국의 pulmonologist는 약 처방시 delivery burden (formulation and frequency)를 중요한 요소로 생각함.
- 환자의 compliance의 중요성에 대해서는 두 지역 모두 SAE 발생 비율보다 더 중요하다고 평가하였음.
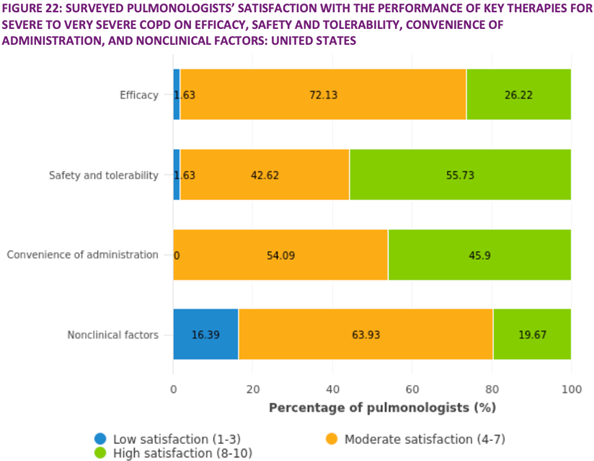
3. Unmet Need in Severe to Very Severe COPD and Related Indications
- Severe to very severe COPD 환자에 대한 치료는 일반적으로 안정성과 tolerability가 efficacy보다 더 중요하다고 여겨짐.
- Efficacy에 대한 unmet need가 높은 것은 현재까지 severe to very severe COPD 환자에 대한 efficacy에 대한 만족도가 낮기 때문임.
- Exacerbation rate의 감소는 미국, 유럽 지역에서 매우 중요한 unmet need로 작용한다.
- 낮은 delivery burden은 중간 수준의 unmet need를 가진다.
- SAE은 unmet need는 높지 않음.
4. Key Findings: Unmet Need in Severe to Very Severe COPD and Related Indications
4.1. Therapy needs that can lead to greater reduction in exacerbation rate.
- 악화 발생률을 줄이기 위한 효과를 보기 위한 임상연구가 진행되고 있음.
>LABA/LAMA/ICS와 meplizumab, benralizubal, dupilumab
> IL-5 inhibitor 및 IL-13/4 inhibitor의 eosinophilic COPD cohort 연구
4.2. Therapy needs that can improve lung function compared with current therapy.
- FEV1은 COPD 약물에 대한 임상 II, III의 primary endpoint로 FDA의 유일한 검증된 지표임.
- RPL554 (PDE3/4 inhibitor)는 임상 2상에서 폐 기능 개선 효과를 보여주었지만 아직 임상 3상 시험이 남아있음.
4.3. Therapy that Can Halt Disease Progression, Reduce Daily Symptoms, and Improve Quality of Life
1) 증상과 QOL을 개선할 수 있는 항염증제는 매력적인 기회가 될 수 있음.
•아직까지 COPD 치료가운데 염증에 효과적인 작용을 가지는 것은 없음.
•COPD 환자의 폐 염증은 질병을 진행을 유도하고 irreversible airfllow obstruction을 유도하지만, inhaled theraphy는 효과적으로 염증에 작용하지 못하고 있음.
•현재 PDE-4 inhibitor인 Roflumailast이 유일하게 함염증제로 사용되고 있지만 위장 부작용에 의해 크게 제한됨.
2) IL-13/4 inhibitor and IL-5 inhibitor가 임상 3상에서 성공한다면 말기 치료제로 사용이 가능할 것이다.
•IL-5 inhibitor의 경우는 eosinophilic asthma population에 효과적이지만, COPD에서는 아직 불명확함.
•Benralizumab은 중요한 2개의 임상 3상 시험을 실패했고, mepolizumab은 3상 한 개에서 에서 primary endpoint를 만족시킴.
•Dupliumab (IL-13/4 inhibitor)의 경우는 아직 COPD에서 효과가 증명된 것이 없음. (eosinophilic asthma population에서는 효과 있음)
5. Assessing Drug Development Opportunities
- Improvement in trough FEV1 at 52 weeks (placebo-adjusted).
- Reduction in frequency of exacerbations over 52 weeks (% reduction, placebo-adjusted).
- QOL improvement at 12 weeks (% patients with SGQR score gain of 4+, placebo-adjusted).
- Improvement in exercise endurance at 6 weeks (%, placebo-adjusted).
- Time on market.
- Delivery burden (formulation and frequency).
• TPP1: triple inhaler commonly prescribed to very severe patients.
• TTP2: mirror the nebulized PDE3/4 inhibitor ensifentrine, which has demonstrated promising efficacy in Phase II clinical trials.→ improve FEV1 at 120ml→TTP1보다 efficacy 좋음.
• TPP3: hypothetical biologic offering improved efficacy on reduction in frequency of exacerbations (30% reduction [TPP 3] versus 15% reduction [TPP 1]) and efficacy on all other efficacy endpoints similar to TPP 1.
- 악화 횟수 감소율이 좋고, efficacy는 유사한 경우
- TPP1이 다른 시나리오보다 더 선호됨. TPP2보다 delivery route가 더 좋고, TPP3보다 가격적으로 낮기 때문이다.
- TPP2의 경우 exacerbation frequency를 15%→30% 향상된 경우는 TTP1보다 더 선호됨→약효가 좋다면 delivery 방법은 바꿀 의향이 있음.
- TPP3의 경우는 excerbation frequency 38% 감소와 FEV1 180ml 향상, QOL 20% 증가해야 가장 선호하는 약물이 될 수 있음. 이것은 biological agent의 프리미엄 가격을 받기 위해서는 효과에 대해 multiple endpoint를 달성해야 하고, excerbation만으로는 프리미엄 가격을 받기는 어렵다는 것을 보여준다.
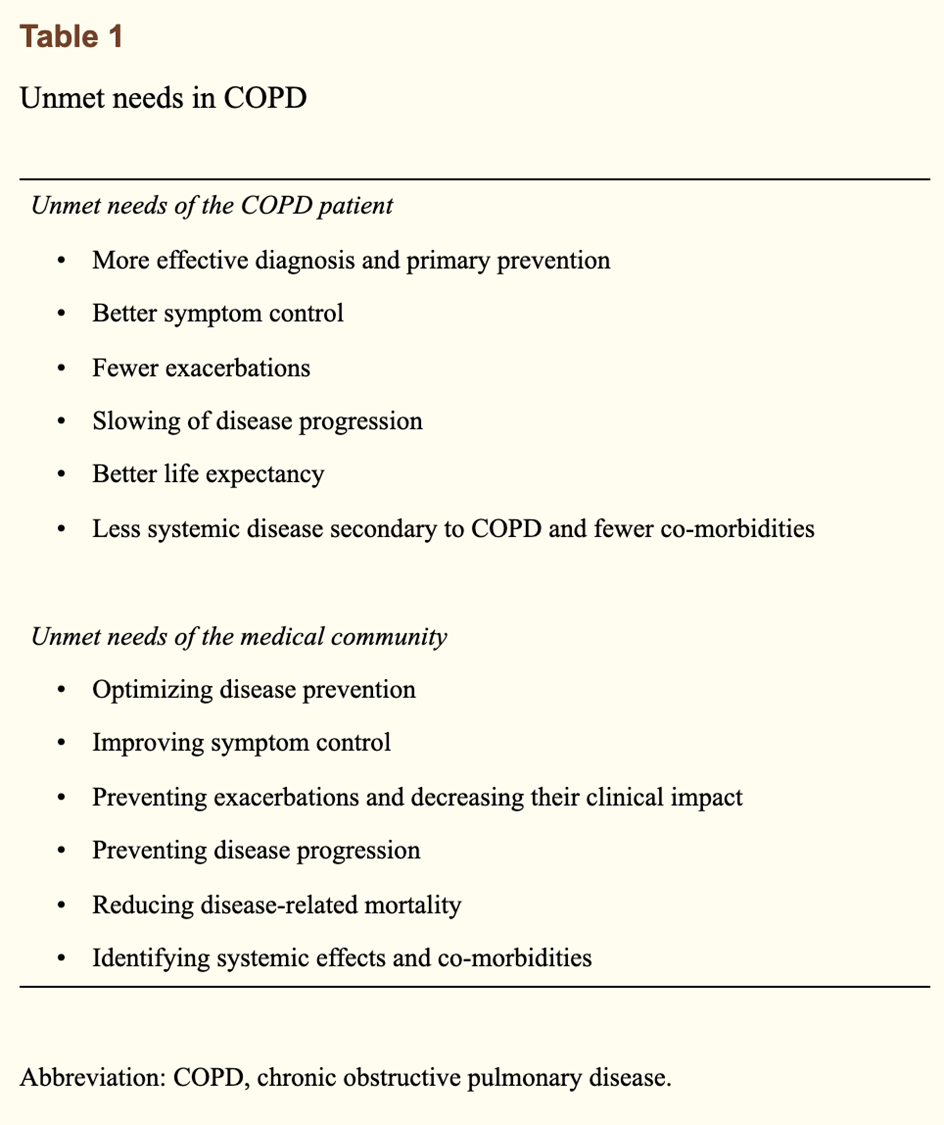
Unmet needs in COPD