현재까지 알려진 COPD biomarker 모음
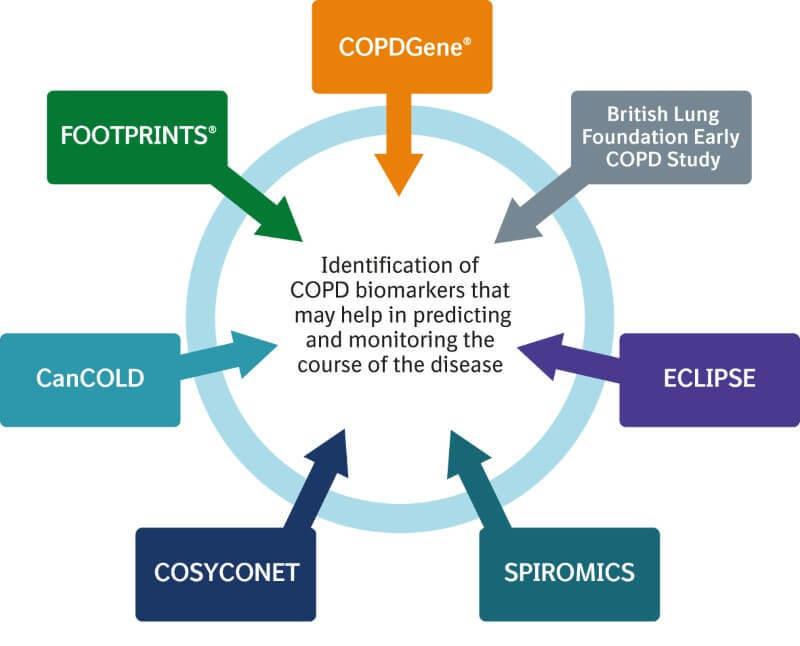
COPD를 평가하는 surrogate biomarker가 마땅한 게 없는 상황이라 COPD 치료제 개발에도 어려움을 주고 있습니다. 하지만 다양한 논문과 빅파마에서 대량의 임상시험을 통해서 바이오마커를 개발하기 위한 노력을 하고 있습니다. 저도 결과가 빨리 나오길 기대하고 있지만 검증까지 언제 완료되나 걱정입니다. 지금까지 나온 COPD 바이오 마커를 정리해봤습니다.
중요한 것은 바이오마커라고 해도 어떤 것과 연관된 바이오마커인지 고려돼야 합니다. 그리고 어느 샘플에서 채취가 가능한지도 확인하면 좋을 것 같습니다.
1. Micro vascular blood flow ( related with lung structure)
Recent publications suggest that early structural alterations of lung parenchyma result in impaired gas exchange and perfusion already before these changes can be detected in high-resolution CT [R19-1222, R19-1219]. Therefore, it is hypothesized that perfusion parameters are sensitive to early structural alterations in the lung and that altered perfusion may be applied to predict the effect of drug intervention on emphysema progression. Lung perfusion can be assessed by dynamic contrast-enhanced magnetic resonance imaging (MRI).
2. SP-D/sRAGE (related with lung density)
There was a significant association between circulating levels of the biomarkers surfactant protein D (SP-D) and soluble receptor for advanced glycation endproduct (sRAGE) with both baseline lung density and its decline over time.
3. CES-D (related with Inflammation)
Mean CES-D score was higher among patients with persistent inflammation than patients without (p = 0.002). At 36 months, CES-D scores were comparable between patients with and without inflammation (p = 0.21). In patients with and without inflammation, changes in CES-D score were also comparable (p = 0.06).
4. C6M (related with Inflammation)
Fidelta study (352.2069) a moderate association has been observed between C6M, a collagen 6 degradation biomarker and lung density as assessed by CT supporting potential utility of this biomarker to monitor tissue destruction and possibly treatment effects on this.
5. 25(OH)D, VDBP (related with FEV1)
For both 25(OH)D25(OH) D and VDBP, a range of serum levels were observed. A significant inverse association was observed between VDBP and FEV1 and 25(OH) D (p = 0.01) and a direct correlation between 25(OH) D and FEV1% predicted.
Vitamin D (hydroxyvitamin D, 25 [OH] D) & FEV1; FEV1 was significantly associated with serum 25(OH) D. Emphysema negatively correlated with serum 25(OH)D.
6. Functional Small Airway Disease (related with lung function)
In two longitudinal observational studies, COPDGene and SPIROMICS, it could be demonstrated that lung regions with fSAD at baseline transitioned into emphysema at follow-up [COPDGene unpublished data, R19-1221]. Recently, it was shown that a higher extent of fSAD is associated with a more rapid decline in FEV1 in healthy smokers and mild to moderate COPD patients. (Diagnostic, prognosis marker?)
7. IL-8 (related with lung inflammation)
IL-8 is a pro-inflammatory cytokine produced by airway epithelial cells and inflammatory cells. It acts as a chemo-attractant, recruiting neutrophils into the lung and thereby causing neutrophil infiltration of the airways. IL-8 potentiates several neutrophil functions.
8. Eosinophils, Neutrophils, lymphocyte, macrophages, Basophils, Cytokine (related with lung inflammation)
A weak association between % sputum neutrophils and FEV1 % were predicted (p < 0.05). Similar weak but significant associations were observed between neutrophil % and health status measured using the St Georges Respiratory Questionnaire. No association was determined between neutrophils and exacerbation rates or emphysema. Non-significant or similarly weak associations were determined between sputum neutrophils and systemic biomarkers. The mean change over 1 year in neutrophil % was an increase of 3.5%.
9. Calprotectin (related with lung inflammation)
Calprotectin is released by neutrophils upon activation and is sputum-independent. In case the NE i treatment leads to a reduced mucus production, such that a relevant proportion of patients lose their ability to produce sputum at the end of the trial, this could make the analysis of sputum endpoints impossible. In this situation, a signal in serum calprotectin would still enable to show an anti-inflammatory effect of NE inhibition.
10. PARC/CCL-18 (related with mortality)
PARC/CCL-18 & total mortality; High levels of serum PARC/CCL-18 were observed in subjects with COPD than in smokers or lifetime nonsmokers without COPD (p < 0.0001). PARC/CCL-18 levels were elevated with total mortality in the ECLIPSE cohort. (원래는 PARC/CCL18은 염증마커)
11. Fibrinogen (related with COPD severity)
Fibrinogen was the most repeatable biomarker. Fibrinogen exhibited a weak correlation with 6-min walk distance, exacerbation rate, BODE index and MRC dyspnoea score in COPD subjects.
12. CRP /fibrinogen /IL-6 /SP-D (related with COPD with exacerbation)
CRP, fibrinogen, interleukin-6 and surfactant protein-D were significantly elevated in those COPD subjects with exacerbations within 30 days of the 3-month visit compared with those individuals that did not exacerbate or whose exacerbations had resolved.
13. % LAA(related with COPD with Emphysema severity)
The percent low attenuation area(% LAA) & visual score of emphysema severity; There was a correlation between the percent low attenuation area (%LAA) and visual scores of emphysema severity (p < 0.001). %LAA, low attenuation cluster analysis, and absence of radiologist described gas trapping, distribution, and predominant type of emphysema were predictors of visual scores of emphysema severity (all p < 0.001). CT scans were scored as showing regions of gas trapping. These regions of gas trapping had smaller lesions for a similar %LAA than those without.
14. CC-16 (related with COPD severity)
In former smokers, with COPD low serum CC-16 levels were determined with increasing severity of COPD (p = 0.006) with forced expiratory volume in 1 s, p < 0.001). But significantly higher levels were determined if they also had reversible airflow obstruction (p = 0.034).
serum CC-16 levels are reduced in individuals with COPD and there is a weak correlation with disease severity in former smokers.
15. DES/IDES or collagen/ elastin fragment (related with lung density)
A correlation of DES/IDES with lung density on CT has so far only been demonstrated in A1 ATD patients in the RAPID trial [R15-3607]. Such correlation could not yet be established in COPD [R19-1215].
16. Lung function, exercise capacity, fibrinogen, BMI (related with mortality)
Lung function, exercise capacity, fibrinogen, BMI & Mortality; Lung function, exercise capacity, fibrinogen and BMI showed a significant association with mortality (p < 0.05).
17. Exacerbation rate (related with COPD severity)
Exacerbation rate & the severity of COPD; As the severity of COPD increased, exacerbations became more frequent. Exacerbation rates in the first year of follow-up were 0.85, 1.34 and 2.00 per person for patients with stage 2, 3 and 4 COPD, respectively. Overall, 22, 33 and 47% of patients with stage 2, 3 and 47% with stage 4 had frequent exacerbations
1. Physiological Response Biomarkers
- Inflammation: Differential cell count in sputum과 hsCRP, WBC, IL-6 plus Fibrinogen을 통해 CatC inhibition을 확인.
- ECM, tissue degradation: DES/IDES, collagen/elastin fragments
- Microvascular blood flow
- RNA sequencing
2. Disease Modulation Biomarkers
- Lung density via CT
- Functional small airway disease: fSAD may potentially be used to select patients that are more likely to progress during the anticipated duration of ph II
- sRAGE: sRAGE (soluble Receptor for Advanced Glycation End products) levels were associated with emphysema. circulating sRAGE levels were significantly associated with emphysema progression